Bursitis Of The Foot Treatments
Bursitis is an inflammation of a bursa. The heel has three areas that are involved in bursitis. Retrocalcaneal Bursa which is located between the Achilles tendon and heel bone. Subcutaneous calcaneal bursa which is located between the skin and where the Achilles tendon attaches to the heel bone. Plantar-calcaneal bursitis is located between the heel bone and the plantar fascia (thick fibrous tissue that inserts into the heel bone).
Causes
The inflammation of a bursa can result from any process that irritates or compresses it. The irritation causes the affected bursa to produce too much fluid and swell. In cases of traumatic injury, injured capillaries can leak blood into the bursa and cause it to swell.
Symptoms
Posterior heel pain is the chief complaint in individuals with calcaneal bursitis. Patients may report limping caused by the posterior heel pain. Some individuals may also report an obvious swelling (eg, a pump bump, a term that presumably comes from the swelling's association with high-heeled shoes or pumps). The condition may be unilateral or bilateral. Symptoms are often worse when the patient first begins an activity after rest.
Diagnosis
To begin with, your doctor will gather a medical history about you and your current condition and symptoms. He/she will inquire about the level of your heel pain, the how long you have had the symptoms and the limitations you are experiencing. Details about what and when the pain started, all are very helpful in providing you with a diagnoses of your ankle / heel.
Non Surgical Treatment
Relieving the symptoms of bursitis initially focuses on taking the pressure off the bursa. This can be done with proper cushioning, inserts, or footwear but may require surgery if it is a bone formation problem (i.e. Huglund's Deformity). If your bursitis is caused by an infection (septic bursitis), the doctor will probably drain the bursa sac with a needle and prescribe antibiotics to treat the infection.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.
Do Hammertoes Hurt
 Overview
Overview
A hammertoe is a toe that is bent because of a weakened muscle. The weakened muscle makes the tendons (tissues that connect muscles to bone) shorter, causing the toes to curl under the feet. Hammertoes can run in families. They can also be caused by shoes that are too short. Hammertoes can cause problems with walking and can lead to other foot problems, such as blisters, calluses, and sores. Splinting and corrective footwear can help in treating hammertoes. In severe cases, surgery to straighten the toe may be necessary.
Causes
The cause of hammertoes varies, but causes include genetics, arthritis and injury to the toe. Treatment for hammertoes depends on the severity and can include anti-inflammatory medication, metatarsal pads, foot exercises and Hammer toes better-fitting shoes. If the pain caused by a hammertoe is so severe that wearing a shoe is uncomfortable, surgery may be necessary. Typically this surgery is an outpatient procedure that doesn?t require general anesthesia, though it is an option. Recovery from surgery usually takes a few weeks, and patients are given special shoes to wear.
 Symptoms
Symptoms
Here is a look at some of the symptoms hammertoe can cause. They include hammer-like or claw-like appearance of the toe. Pain when walking or moving the foot. Difficulty moving the toe. Corns may form on top of the toe. Callus may form on the sole of the foot. During the initial stages, you may be able to manually straighten your toe. This is called a flexible hammertoe. But as time passes, the toe will not move as easily and will continue to look like a hammer. Pressure and irritation over the joint can cause a blister to develop and become a corn over time. These corns have the potential to become infected and cause additional symptoms such as redness, bleeding, and difficulty wearing shoes and socks. Corns are the main cause of pain when hammertoes are developing.
Diagnosis
The earlier a hammertoe is diagnosed, the better the prognosis and treatment options. Your doctor will be able to diagnose your hammertoe with a simple examination of the foot and your footwear. He or she may take an x-ray to check the severity of the condition. You may also be asked about your symptoms, your normal daily activities, and your medical and family history.
Non Surgical Treatment
What will a doctor do? Treat any foot complaints such as corns, calluses by periodically reducing the lesion and applying appropriate pads and dressings. Recommend the silicone toe prop. If an infection is present, then anti-septic dressings, antibiotics and pads to redistribute pressure away from the lesion may be necessary. In the case of a mallet toe, trigger toe or claw toe. If a corn occurs at the end of the toe, a silicone or leather prop may be used to straighten the toe. In a hammertoe deformity, a silicone prop to redistribute pressure away from a corn may be necessary. The doctor may give footwear advice. In severe cases, corrective surgery may be necessary. The doctor may recommend orthosis to correct a mechanical complaint of the foot, such as 3/4 length silicone insoles.
Surgical Treatment
Extreme occurrences of hammer toe may call for surgery. Your surgeon will decide which form of surgery will best suit your case. Often, the surgeon may have to cut or remove a tendon or ligament. Depending on the severity of your condition, the bones on both sides of the joint afflicted may need to be fused together. The good news is you can probably have your surgery and be released to go home in one day. You will probably experience some stiffness in your toe, but it might last for a short period, then your long-term pain will be eliminated.
 Prevention
Prevention
To help prevent hammer toes from developing, wear shoes or boots that provide sufficient width in the toe box to ensure minimal compression. Use inserts that help the toes flatten out and spread and give sufficient support to the metatarsal arch in the forefoot. If hammer toes have already formed, padded socks help protect the tops and the tips of the hammer toes and may reduce pain from rubbing and chafing.
Hammer Toe Leading To Ball Of Foot Pain
 Overview
Overview
hammertoe is often a harmless and painless condition. Although the toe may be curled permanently, hammertoe should not cause any long-term problems other than a more difficult time finding shoes that fit. If hammertoe is treated and preventive measures are followed, the condition should not return. Wearing tight or constricting shoes can cause hammertoe to return.
Causes
Claw, hammer and mallet toe are most commonly caused by wearing high heels or ill-fitting shoes that are too tight e.g. narrow toebox. If shoes like this are worn for long periods, the foot is held in a slightly bent position and gradually over time, the muscles tighten and shorten. If this continues for long enough, then the muscles become so tight that even when shoes are removed, the toe is still held in the bent position. Another common cause is Morton?s Toe, where the second toe is longer than the big toe. In this case, the second toe is commonly squashed into a shoe into an unnaturally bent position.
 Symptoms
Symptoms
If the toes remain in the hammertoe position for long periods, the tendons on the top of the foot will tighten over time because they are not stretched to their full length. Eventually, the tendons shorten enough that the toe stays bent, even when shoes are not being worn. The symptoms of hammertoe include a curling toe, pain or discomfort in the toes and ball of the foot or the front of the leg, especially when toes are stretched downward, thickening of the skin above or below the affected toe with the formation of corns or calluses, difficulty finding shoes that fit well. In its early stages, hammertoe is not obvious. Frequently, hammertoe does not cause any symptoms except for the claw-like toe shape.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
A number of approaches can be undertaken to the manage a hammer toe. It is important that hammertoes any footwear advice is followed. The correct amount of space in the toe box will allow room for the toes to function without excessive pressure. If a corn is present, this will need to be treated. If the toe is still flexible, it may be possible to use splints or tape to try and correct the toe. Without correct fitting footwear, this is often unsuccessful. Padding is often used to get pressure off the toe to help the symptoms. If conservative treatment is unsuccessful at helping the symptoms, surgery is often a good option.
Surgical Treatment
If this fails or if treatment is not sought until the toes are permanently misaligned, then surgery may be required. Surgery may involve either cutting the tendon or fusing the joint. Congenital conditions should be treated in early childhood with manipulations and splinting.
The Truth About Over-Pronation Of The Feet
Pronation describes the natural process of the inward rolling of your foot when the outer edge of your heel strikes the ground and your foot flattens out. Excess pronation, known as flat foot, can result in flattened arches and overstretched foot muscles. Advanced conditions may affect your hips, knees, ankle, back and foot functioning. Use natural techniques to stretch and strengthen your muscles in order to help pronation.

Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding stress to other parts of the foot. As a result, over-pronation, often leads to Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Because overpronation affects the entire lower leg, many injuries and conditions may develop and eventually cause problems not only in the leg and foot, but also the knee, hips and lower back. Pain often begins in the arch of the foot or the ankle. Blisters may develop on the instep, or on the inside edge of the heels. As overpronation continues and problems develop, pain will be felt elsewhere, depending on the injury.
Diagnosis
Do the wet foot test. Get your feet wet and walk along a paved surface or sand and look at the footprints you leave. If you have neutral feet you will see a print of the heel with a thin strip connecting to your forefoot, but if you're overpronating your foot print will look a bit like a giant blob with toes.

Non Surgical Treatment
Side Step with Opposite Reach. This exercise is designed to load the "bungee cord system" of the gluteal muscle and its opposite, latissimus dorsi muscle to keep the foot from overpronating. Because the opposite arm swings across the front leg when walking, this exercise creates tension in the muscles all the way from the front foot, across the back of the hips and back, to the fingers of the opposite hand. Movement Directions. Stand with left foot on top of the dome of the BT. (Note: For added balance, the right foot can tap on the ground, if needed). Reach right leg out to the side of the BT, and tap the ground while squatting down on the left side and reaching right arm across the left knee. Push down with left big toe while squatting. This activates the arch of the left foot and strengthens all the stabilizing muscles on the left side of the lower body. Return to starting position. Perform 8 to 10 repetitions on each leg.
Surgical Treatment
Subtalar Arthroereisis. The ankle and hindfoot bones/midfoot bones around the joint are fused, locking the bones in place and preventing all joint motion. This may also be done in combination with fusion at other joints. This is a very aggressive option usually reserved for extreme cases where no joint flexibility is present and/or the patient has severe arthritic changes in the joint.
How To Get Rid Of Bunions On Feet
Overview
 A bunion (hallux abducto valgus) is a bony lump or enlargement that forms in the joint (metatarsal phalangeal joint) at the base of the big toe. The big toe points toward the other toes (lateral deviation) as the bunion progresses. The joint and surrounding tissue becomes inflamed and painful. Occasionally bunions can also form at the joint at the base of the smallest (fifth) toe. They are called a tailor's bunion or bunionette. Bunions can be accompanied by bursitis (inflammation of a small fluid-filled sac adjacent to the joint). With an advanced bunion the big toe may be so deformed that it has to lie over or under the second toe. In this situation it hurts to walk or wear any kind of shoe. About one in three people in most Western countries will get a bunion. They are about ten times more common in women than in men. Older people are more often affected than younger people, although bunions do occur in children with misaligned feet. Bunions should not be confused with gout or arthritis, which can also cause inflammation, deformity and pain around the toes and feet.
A bunion (hallux abducto valgus) is a bony lump or enlargement that forms in the joint (metatarsal phalangeal joint) at the base of the big toe. The big toe points toward the other toes (lateral deviation) as the bunion progresses. The joint and surrounding tissue becomes inflamed and painful. Occasionally bunions can also form at the joint at the base of the smallest (fifth) toe. They are called a tailor's bunion or bunionette. Bunions can be accompanied by bursitis (inflammation of a small fluid-filled sac adjacent to the joint). With an advanced bunion the big toe may be so deformed that it has to lie over or under the second toe. In this situation it hurts to walk or wear any kind of shoe. About one in three people in most Western countries will get a bunion. They are about ten times more common in women than in men. Older people are more often affected than younger people, although bunions do occur in children with misaligned feet. Bunions should not be confused with gout or arthritis, which can also cause inflammation, deformity and pain around the toes and feet.
Causes
The commonest cause of bunions is prolonged wearing of poorly designed shoes such as the narrow high heels that women wear. This is one of the reasons why bunions are much more common in women than in men. There is also a hereditary component to bunions in that many times we will see a grandmother, mother and daughter all with various stages of bunions. 38% of women in the United States wear shoes that are too small and 55% of women have some degree of bunion formation. Bunions are 9 times more common in women than they are in men.
Symptoms
Symptoms include redness, swelling and pain which may be present along the inside margin of the foot. The patients feet may become too wide to fit into their normal size shoes and moderate to severe discomfort may occur when the patient is wearing tight shoes. A "hammer toe" may occur at the 2nd toe. This is when the toe contracts and presses on the shoe. Subsequently, this may cause a corn on top of the 2nd toe.
Diagnosis
When an x-ray of a bunion is taken, there is usually angulation between the first metatarsal bone and the bones of the big toe. There may also be angulation between the first and second metatarsal bones. These angular irregularities are the essence of most bunions. In general, surgery for bunions aims to correct such angular deformities.
Non Surgical Treatment
Your podiatrist can recommend exercises, orthoses (special devices inserted into shoes), shoe alterations or night splints (which hold toes straight over night) which may slow the progression of bunions in children. According to experts, ?conservative? measures such as these may help relieve symptoms, though there is no evidence they can correct the underlying deformity. Orthoses are designed to prevent the problem getting worse by decreasing any biomechanical causes of bunions. In other words, if the biomechanical theory is correct (i.e. if your bunions are caused by the way you walk), orthoses may help you walk in a way that doesn?t exacerbate the problem. But it won?t change the already established shape of your foot. For that, you need surgery. 
Surgical Treatment
Depending on the size of the enlargement, misalignment of the toe, and pain experienced, conservative treatments may not be adequate to prevent progressive damage from bunions. In these cases, bunion surgery, known as a bunionectomy, may be advised to remove the bunion and realign the toe.
Prevention
Choosing footwear that fits correctly, especially low heeled shoes with plenty of space for the toes, is one of the main ways that bunions can be prevented. Always stand when trying on shoes to ensure they still fit comfortably when the foot expands under your body weight. Try shoes on both feet, and select the size appropriate for your larger foot. Use an extra insole if one shoe is looser than the other. Do not cramp the larger foot. People prone to flat-footedness should consider the use of arch supports, orthotic shoe inserts or special orthotic shoes to prevent or delay the development of bunions.
Coping With Severs Disease
Sever's disease is the most common cause of heel pain in the growing child. It is due to overuse and repetitive stress of the Achilles tendon where it attaches to the heel bone.
Causes
The condition generally occurs in active children at early adolescence during rapid growth periods as the heel bone can grow faster than the leg muscles causing them to become tight and overstretched. Sever?s disease most often caused by inadequate footwear, playing sport on hard surfaces, calf tightness and biomechanical problems.
Symptoms
Severs causes swelling, pain and tenderness over the back of the heel. Your child may walk with a limp. Initially the pain may be intermittent occurring only during or after exercise. As the problem gets worse, pain may be present most of the time. The swelling increases and is painful when touched or knocked. It commonly affects boys who are having a growth spurt during their pre-teen or teenage years. One or both knees may be affected.
Diagnosis
Low-grade inflammation of the calcaneal apophysis cannot be seen on x-ray. Therefore, although x-rays are often done to rule out bony injuries in children with Sever's disease these x-rays are usually normal. Advanced Sever's disease can be seen on x-ray but usually the problem is treated before it reaches this point. Other diagnostic tests, such as bone scans or MRI's, are not usually required in typical cases of Sever's disease. These, or other tests, may be required to rule out other conditions, such as stress fractures of the calcaneus or other bony abnormalities that can mimic Severs disease.
Non Surgical Treatment
Initially, treatment will consist of resting from activity, ice and anti-inflammatory medications to reduce the pain. Your physiotherapist may also use a variety of pain reducing techniques such as soft tissue massage or joint mobilisations. They may recommend taping to unload the area of pain, heel cups or wedge inserts into the bottom of your shoe. Also in the initial phase we may also refer you to podiatry for orthotics and/or further footwear recommendations. It is also ideal in the first instance to start stretching your calf muscles and achilles. This initial phase typically lasts for 1-2 weeks. During this time your physiotherapist will guide you on appropriate levels of activity- they may recommend you rest from impact type activities during this phase, and will guide you on the best program to return to your sport without any further injury.
Recovery
One of the most important things to know about Sever's disease is that, with proper care, the condition usually goes away within 2 weeks to 2 months and does not cause any problems later in life. The sooner Sever's disease is addressed, the quicker recovery is. Most kids can return to physical activity without any trouble once the pain and other symptoms go away. Although Sever's disease generally heals quickly, it can recur if long-term measures are not taken to protect the heel during a child's growing years. One of the most important is to make sure that kids wear proper shoes. Good quality, well-fitting shoes with shock-absorbent (padded) soles help to reduce pressure on the heel. The doctor may also recommend shoes with open backs, such as sandals or clogs, that do not rub on the back of the heel. Shoes that are heavy or have high heels should be avoided. Other preventive measures include continued stretching exercises and icing of the affected heel after activity.
Flat Foot Symptoms In Adults
Overview
Originally known as posterior tibial tendon dysfunction or insufficiency, adult-acquired flatfoot deformity encompasses a wide range of deformities. These deformities vary in location, severity, and rate of progression. Establishing a diagnosis as early as possible is one of the most important factors in treatment. Prompt early, aggressive nonsurgical management is important. A patient in whom such treatment fails should strongly consider surgical correction to avoid worsening of the deformity. In all four stages of deformity, the goal of surgery is to achieve proper alignment and maintain as much flexibility as possible in the foot and ankle complex. However, controversy remains as to how to manage flexible deformities, especially those that are severe. 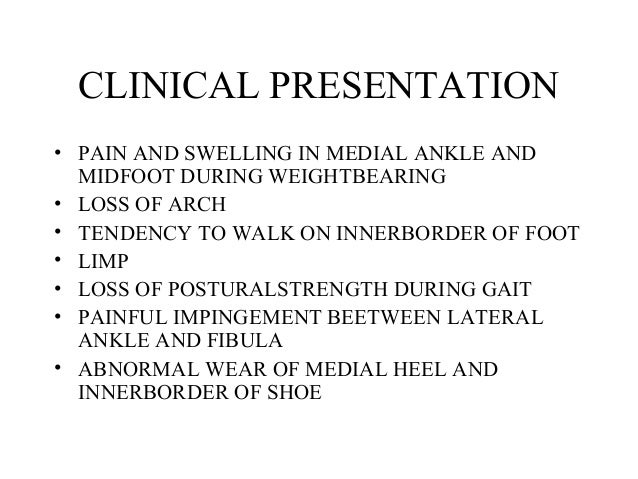
Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms here. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Diagnostic testing is often used to diagnose the condition and help determine the stage of the disease. The most common test done in the office setting are weightbearing X-rays of the foot and ankle. These assess joint alignment and osteoarthritis. If tendon tearing or rupture is suspected, the gold standard test would be MRI. The MRI is used to check the tendon, surrounding ligament structures and the midfoot and hindfoot joints. An MRI is essential if surgery is being considered.
Non surgical Treatment
Nonoperative treatment of posterior tibial tendon dysfunction can be successful with the Arizona AFO brace, particularly when treatment is initiated in the early stages of the disease. This mandates that the orthopedist has a high index of suspicion when evaluating patients to make an accurate diagnosis. Although there is a role for surgical management of acquired flat feet, a well-fitted, custom-molded leather and polypropylene orthosis can be effective at relieving symptoms and either obviating or delaying any surgical intervention. In today's climate of patient satisfaction directed health care, a less invasive treatment modality that relieves pain may prove to be more valuable than similar pain relief that is obtained after surgery. Questions regarding the long-term results of bracing remain unanswered. Future studies are needed to determine if disease progression and arthrosis occur despite symptomatic relief with a brace. Furthermore, age- and disease stage-matched control groups who are randomized to undergo surgery or bracing are necessary to compare these different treatment modalities. 
Surgical Treatment
If conservative treatments don?t work, your doctor may recommend surgery. Several procedures can be used to treat posterior tibial tendon dysfunction; often more than one procedure is performed at the same time. Your doctor will recommend a specific course of treatment based on your individual case. Surgical options include. Tenosynovectomy. In this procedure, the surgeon will clean away (debride) and remove (excise) any inflamed tissue surrounding the tendon. Osteotomy. This procedure changes the alignment of the heel bone (calcaneus). The surgeon may sometimes have to remove a portion of the bone. Tendon transfer: This procedure uses some fibers from another tendon (the flexor digitorum longus, which helps bend the toes) to repair the damaged posterior tibial tendon. Lateral column lengthening, In this procedure, the surgeon places a small wedge-shaped piece of bone into the outside of the calcaneus. This helps realign the bones and recreates the arch. Arthrodesis. This procedure welds (fuses) one or more bones together, eliminating movement in the joint. This stabilizes the hindfoot and prevents the condition from progressing further.